Will the UK see medical cannabis prescribed instead of expensive and more damaging opioid drugs
A recently published white paper on medical cannabis from the Journal of Psychopharmacology has been produced and published recently presenting essential points on prescription of medical cannabinoids. See our exhibit 1 below for the 2019 value of the total cannabis market recreational and medical by region.
Exhibit 1 Global cannabis demand 2019 in USD bn by region
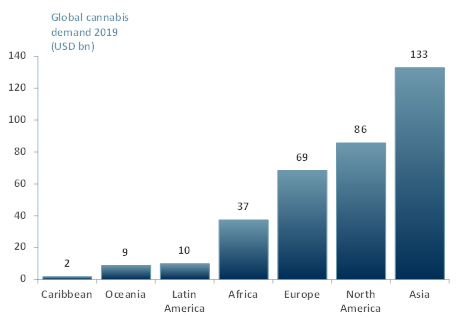
Source: ACF Equity Research; New Frontier Data
- The white paper examined the question of how to optimise clinical research but also how to ethically improve patient access.
- The paper offered potential solutions to help the medical profession respond to growing demand for medical cannabis and prescribe it, despite an as yet limited scientific evidence-base on the efficacy of medical cannabis.
- There is a growing demand for medical cannabis but there is a constriction at the distribution point i.e. with prescribers. The white paper argues that the prescriber issue is in need of significant review.
- In the UK, cannabis was made a medicine on the 1st of November 2018, nevertheless medical cannabis remains unavailable to most potential patients. Less than 60 prescriptions have been issued so far in the UK market (definitions and to numbers are disputed so we restrict this discussion to full extract medical cannabis only).
- The lack of prescriptions is largely due to prescriber resistance underpinned by a lack of knowledge on the science itself and also low awareness of the cost of prescribing despite medical cannabis being the potential solution for reducing the use of costly (cash and to society) opioid medicines.
- The main challenge is education. Medical schools need to update their curriculums to include medical cannabis, medical doctors (MDs) do not prescribe in general something they do not comprehend or recognise.
- There is a much-needed effort to educate medical practitioners and persuade them to accelerate the integration of medical cannabis into UK practitioner healthcare programmes.
- Small scale training programmes through the Medical Cannabis Clinicians Society (MCCS) have been offered, but each medical school has its own education and training agenda and medical cannabis is not yet a curriculum subject.
- Another factor that has slowed down the prescribing is the negative guidelines produced by the National Institute for Health & Care in the UK (NICE). The prescription of medical cannabis is currently only supported by NICE’s guidelines in exceptional circumstances until there is more scientific and social evidence.
- NICE set its standards based on double-blind trials and placebo-controlled studies into which MC does not fit.
- Each patient needs a different prescription because medical cannabis is a botanical product and with a large extended family of cannabinoids and terpenes and concentrations of the active ingredients and their ratios change between varieties and crops (much like any soft commodity).
- It seems clear that there is a need for more scientific research and medical trials, probably largely to build confidence and reduce risk anxiety in MDs and NICE.
ACF view: Cost and accessibility should not be a barrier: Telemedicine would be a huge help with medical doctors’ online consultations and help patients in remote locations. The NHS and NICE must understand that it can actually save them money as medical cannabis can be prescribed instead of, for example, expensive and more damaging opioid drugs.
Overall, the prescription of medical cannabis in the UK will accelerate and improve as all parties – prescribers, clinics, researchers, and patients – can see how cannabis affects patients both short term and longitudinally. Whatever the outcome, education is the first key step for corporates producing, investors investing and physicians wondering.
















