Immune response and catching Covid twice
The Lindsley F. Kimball Research Institute of the New York Blood Centre and Rockefeller University in June concluded that herd immunity is not as simple as it sounds but that antibody testing retains a key role in localised lockdowns. Localised lockdowns have recently become the preferred strategy to contain the SARS-CoV-2 pandemic.
The Rockefeller supported Kimball institute carried out a study that looked at the antibodies produced by people who have recovered from SARS-CoV-2 (Covid-19). It found that only 10% of patients had high enough antibodies to neutralise the virus.
The Kimball NYBC Rockefeller found that whilst 88% of patients sampled generated various levels of antibodies, only 10% had high enough levels to neutralise the virus. A significant proportion of patients in the Kimball study had no antibody response at all.
The Kimball Rockefeller study analysed 370 blood samples from CP donors (CP refers to the ‘convalescent plasma’ transfusions used as a treatment for Covid patients) to test the metrics for herd immunity.
The Kimball Rockefeller researchers used antibody testing methods to observe the levels of immune system antibodies these patients generated against SARS-CoV-2 and they observed whether the antibodies could actually neutralise (or kill) the virus. Due to SARS-CoV-2 having a biosafety level of three and the need for urgency in finding an antibody, researchers used pseudo-type viruses – HIV-1 (human immunodeficiency virus type 1) or VSV (vesicular stomatitis virus).
Immune response pathways
Exhibit 1:Adaptive Immune System
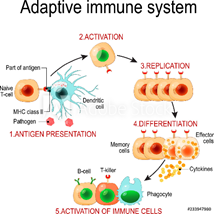
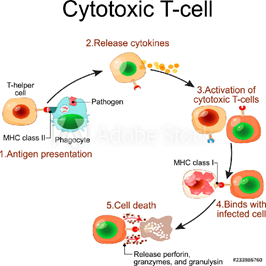
Exhibit 2: Recaps step 5 from Exhibit 1 above and shows the actions leading to cell death after the Cytokines are released
The results indicate that the notion of herd immunity is not as simple as we think. Even though all the patients sampled recovered from Covid, some immune systems showed a strong dependence on antibodies and others relied on different types of cells. Furthermore, doctors should not just test for antibody levels, they should be looking to understand what those levels mean for a patient’s ability to fight off the virus.
Head Kimball Rockefeller researcher Dr. Luchsinger says that the only way to know for sure what level of antibody is required to neutralise a virus would be to take these individuals and re-expose them to that virus i.e. SARS-CoV-2, which of course is highly controversial.
In the meantime, the Kimball Rockefeller study has expanded to match people’s antibody levels with their symptoms to understand how actively or inactively their antibodies behaved based on the severity of the symptoms they experienced.
To make a vaccine that works can take anywhere from 12 to 18 months. Antibody testing will be just as important as vaccines in that people who have low or no antibody level can be prioritised. Antibody testing can also help experts understand how well any vaccines are working.
Given the data above, it still remains unclear, in spite of today’s news that a person caught Covid for a second time, whether or not having an antibody response can stop an individual from getting infected again by SARS-CoV-2. We need more data on the case in the news – e.g. what was the level of antibody response on the first infection, if any.
In spite of yesterday’s news rolling out mass antibody testing in the interim remains one way to prepare for a second wave and if necessary, the ever more popular, localised lockdowns strategy. Antibody testing can also improve the probability of the out of home workplace becoming a safe environment again, which is important to key segments of the economy.
The article speaks to the resilience and importance of the healthcare industry where we see increased value in firms making investment in research and development.
The majority of investors are more inclined to deal with larger healthcare companies because of the lower implied investment risk compared to smaller firms. However, we argue for a change of mindset in which, to some extent, it becomes a duty for 10% of any fund to be allocated to higher risk higher return investing in healthcare and technology. Perhaps this could be an ESG metric investment managers impose upon themselves.
In the UK, for example, there are approx. 100,000 antibody tests available from small firms, however, the UK government is dragging its feet when it comes to purchasing from these firms. The reasoning behind this is a concern as to the efficiency of these tests. As a result, smaller firms are looking to sell their products overseas and are accusing the government of stonewalling their efforts, which seems backward thinking to us.
The healthcare industry has not always shown consistent growth at the individual stock level, but the sector in general has managed to maintain its resilience and probably has the best chance of providing a solution to the SARS-CoV-2 pandemic.
The future of global healthcare systems is dependent on the collaborative efforts of all stakeholders and parties involved (investment firms, small and large cap corporates, and though we are loathed to concede it, governments too).
Affordable and reliable healthcare for all should be a mantra for everyone. Why? Because although it is the compassionate approach, it is also a foundation pillar at the heart of local and global economic success.
Author: Renas Sidahmed – Renas is a Staff Analyst and part of the Sales & Strategy team at ACF Equity Research. See Renas’s profile here
















